Financial Inaccessibility of Mental Healthcare in the United States
Photo by Towfiqu barbhuiya on Unsplash
By Sophie Lasswell
Published Fall 2022
Special thanks to Erica Bassett for editing and research contributions.
Summary+
Despite progressive improvements in healthcare in the United States, healthcare for individuals who experience mental health issues remains financially inaccessible. For this brief, financial inaccessibility refers to an individual’s inability to afford mental healthcare services, such as therapy, prescriptions, and inpatient and outpatient services. Inadequate execution of legislation, such as the Mental Health Parity and the nature of insurance coverage, contribute to inaccessible mental healthcare in the US. Additionally, the United States maintains healthcare and health insurance costs that are more expensive than comparable developed countries, which contributes to the inaccessibility of mental healthcare in the United States. As a result of this social issue, individuals experience poorer mental and physical health outcomes with lifelong impacts. Furthermore, because access to mental healthcare helps to reduce suicide frequency, financial inhibitions to accessing mental healthcare exacerbate suicide rates. Finally, the widespread inaccessibility of mental healthcare contributes to high economic costs nationally and globally, as well as to individual consumers. Efforts such as safety net hospitals, which predominantly serve low-income individuals, may help alleviate this issue. However, due to their financial and resource challenges, safety-net hospitals may not survive in the coming years.
Key Takeaways+
- In 2020, an estimated 52.9 million people had a mental illness in the United States, and estimates predict that 50% of all Americans will have a diagnosable mental illness at some point in their lifetime. 167
- Prices for psychiatric residential treatment facilities range from $10,000.00–$60,000.00 per month. In one study, 42% of untreated Americans reported cost as a barrier to accessing the mental healthcare they needed. 168
- Because insurers can determine medical necessity on a case-by-case basis, limit reimbursement rates, and narrow insurance networks for mental healthcare, individuals requiring mental healthcare are inhibited from accessing mental healthcare services in the United States. 169
- Only 18.3% of individuals who committed suicide had an inpatient mental health stay, only 26.1% acquired outpatient mental health services, and only 25.7% had both inpatient and outpatient mental health services. 170
- Poor mental health and consequentially reduced productivity cost the global economy approximately $2.5 trillion annually in 2010 and will increase to $6 trillion by 2030. 171
Key Terms+
Adverse Benefit Determination—The event wherein a service is denied, postponed, or limited. 1
Affordable Care Act (ACA; also known as Obamacare)—A healthcare reform law established in March 2010. This law is designed with three primary functions in mind: make affordable health insurance available to more people through providing subsidies that lower costs for households with incomes between 100–400% of the federal poverty level; expand the Medicaid program to cover all adults with incomes below 138% of the federal poverty level; support innovative medical care delivery methods directed towards lowering costs of healthcare. 2
Age-Adjusted—“Age-adjusted” data allow populations with different age structures to be statistically compared; this is often applied to health outcomes measurements. 3
Behavioral Health—“Behavioral health refers to mental health, psychiatric, marriage and family counseling and addictions treatment, and it includes services provided by social workers, counselors, psychiatrists, neurologists and physicians, the National Business Group on Health says. Behavioral health includes mental health and substance use, encompassing a continuum of prevention, intervention, treatment, and recovery support services.” 4
Delivery System Reform Incentive Payment (DSRIP)—Contemporary type of supplemental payment program that provides incentive payments for hospitals and other providers to undertake delivery system transformation efforts. 5
Federal Poverty Line (FPL)—The amount of annual income earned by a household below which they would be eligible to receive federal welfare benefits. 6
Health Insurance—The arrangement wherein a company or government agency provides compensation for a specified illness or injury in return for a premium payment. 7
Healthcare—The maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments. 8
Mental Health—The state or condition of one’s emotional and psychological well-being. 9
Outpatient—Outpatient mental healthcare refers to intensive mental health treatment that does not require an inpatient hospital stay; outpatient services provide patients with intensive mental health services while allowing them to return home at night and continue their daily obligations. 10
Parity—The state of being equal or equivalent. 11
Safety Net Hospital—A type of medical center in the United States that, by legal obligation, provides healthcare for individuals regardless of their insurance status or ability to pay; these hospitals typically provide services disproportionately to low-income and marginalized populations. 12
Social Drift—A term used in social epidemiology to describe the downward social mobility of an individual. 13
Social Mobility—The movement of individuals along a social hierarchy. 14
Socioeconomic Status (SES)—The social status or standing of an individual, typically measured by education, income, and occupation. 15
The Mental Health Parity and Addiction Equity Act—United States legislation that requires equal treatment and financing of mental health conditions and substance abuse disorders in insurance plans. 16
Context
Q: Who is most affected by inaccessible mental healthcare in the US?
A: Inaccessible mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 affects individuals who experience mental healthThe state or condition of one’s emotional and psychological well-being.9 issues the most. Mental illnesses represent 4 of the top 10 causes of disability in America, and an estimated 50% of all Americans will have a diagnosable mental illness at some point in their lifetime.17 Many individuals suffer from multiple mental illnesses at a given time, with anxiety and mood disorders as the most common mental illnesses.18 In 2020, an estimated 52.9 million people had a mental illness in the United States.19 Mental illness was higher among females (25.8%) than males (15.8%) and higher among young adults aged 18–25 (30.6%) compared to adults aged 26–49 (25.3%) and adults aged 50+ (14.5%).20
Among racial minorities, severe mental illness was more frequent among multiracial individuals, followed by American Indian or Alaskan Natives, Hispanics, Blacks, and Asians, respectively.21 One study found a higher frequency of depression among Hispanic adults (40.3%) compared to Non-Hispanic white individuals (25.3%), as well as higher rates of suicide ideation (22.9% and 5.3%, respectively).22 The CDC reported that 23% of Non-Hispanic white adults were more likely to have received any mental healthThe state or condition of one’s emotional and psychological well-being.9 treatment compared to 12.9% of Hispanic adults;23 thus, while Hispanic individuals experienced higher rates of depression and suicide ideation than white individuals, they were less likely to have received mental health treatment. Racial stigma and insufficient access to structural determinants (that is, safe housing, healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8, healthy food, and so on) of health can increase the frequency of chronic stress and negatively impact mental and physical health among racial minorities.24 Thus, poor mental health can be more frequent among racial minorities.
Individuals living below the poverty line are more than twice as likely to experience mental healthThe state or condition of one’s emotional and psychological well-being.9 challenges, like depression, than individuals at or above the poverty line—indicating a greater need for mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 among low-income individuals.25 Approximately 8.7% of individuals living below the poverty line reported severe psychological distress.26 The CDC found that as income levels increased, psychological distress decreased; thus, poor mental health negatively correlates with income levels.27 Congruently, studies have shown that rates of depression are unevenly distributed among income levels; for example, depression, dementia, bipolar disorder, and schizophrenia were more common among low socioeconomic strata.28, 29 Individuals with low socioeconomic statusThe social status or standing of an individual, typically measured by education, income, and occupation.15 are subject to greater sources of stress and strain, which create a disproportionately higher risk of developing mental illness.30
Family members and friends are also affected by an individual’s mental illness. As individuals struggle with mental illness, they can become the main focus of their family, which may negatively affect the entire family. Siblings, parents, and friends of a person with mental illness reported feeling angry, resentful, stigmatized, or depressed due to the added strain.31 In a study of 15 family caregiver respondents, 10 reported financial difficulties in supporting their mentally ill family member and 5 responded that they needed to receive financial aid from their other children.32 In this evaluation of the effect of mental illness on family members, many respondents also cited stigma and negative psychological effects.33
Q: What does the mental healthcare system look like in the US?
A: In the United States, various treatment approaches, facility types, and services address mental illness. Treatment for mental and behavioral health“Behavioral health refers to mental health, psychiatric, marriage and family counseling and addictions treatment, and it includes services provided by social workers, counselors, psychiatrists, neurologists and physicians, the National Business Group on Health says. Behavioral health includes mental health and substance use, encompassing a continuum of prevention, intervention, treatment, and recovery support services.”4 issues is typically sought when individuals experience chronic stress, experience inhibitions affecting daily and social functioning, and have various symptoms, such as severe anxiety, excess worry, and depression.34, 35, 36 Treatment may include medication, therapy or counseling, and hospitalizations. In 2019, 19.2% of adults in the United States received mental healthThe state or condition of one’s emotional and psychological well-being.9 treatment during the past 12 months, 15.8% received medication for mental health, and 9.5% received counseling or therapy.37
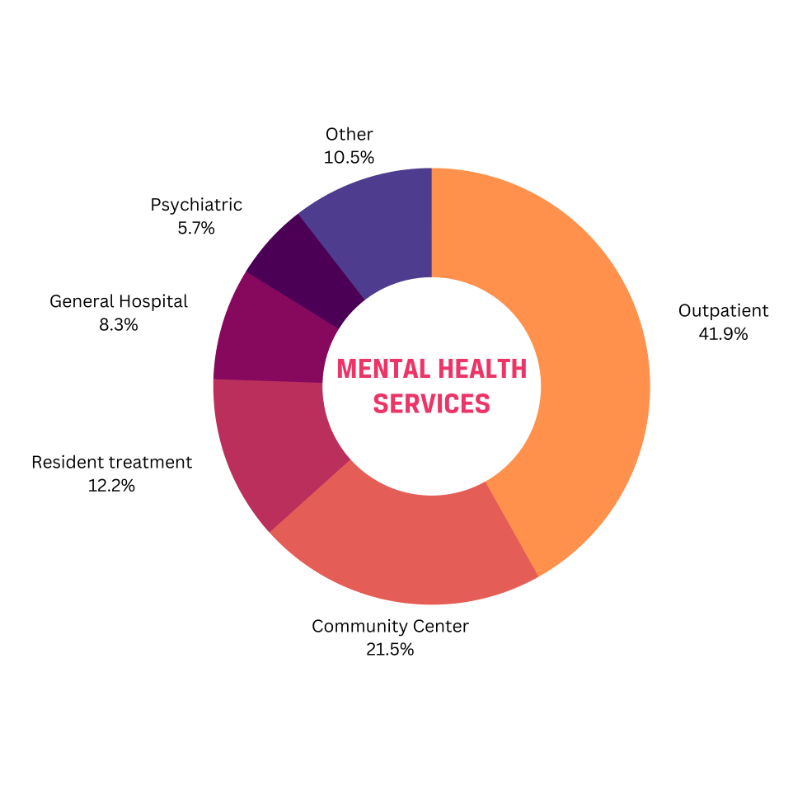
Most facilities that administer mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 are private non-profit organizations (61.1%), while 20.2% are private for-profit organizations.38 Other facilities include regional/local municipal government-run facilities, state mental healthThe state or condition of one’s emotional and psychological well-being.9 agencies, and tribal government facilities. Mental health services include outpatientOutpatient mental healthcare refers to intensive mental health treatment that does not require an inpatient hospital stay; outpatient services provide patients with intensive mental health services while allowing them to return home at night and continue their daily obligations.10 (41.9%), community center (21.5%), residential treatment (12.2%), general hospital (8.3%), psychiatric hospital (5.7%), and other services (10.5%).39
The most common mental healthThe state or condition of one’s emotional and psychological well-being.9 treatment approaches are individual psychotherapy, cognitive behavioral therapy, group therapy, psychotropic medication, family therapy, and behavior modification.40 Cognitive behavioral therapy, for instance, focuses on identifying unhealthy thought patterns and replacing them with healthy ones.41 Studies have shown its effectiveness for many mental illnesses, and brain activity evaluation found that it improves brain functioning.42 HealthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 professionals that provide these services include psychologists, psychiatrists, therapists, counselors, and social workers.
Q: How does this brief define the financial inaccessibility of mental healthcare?
A: “Accessibility” is not consistently defined in existing research, leading to complications in policy and evaluation. Access can revolve around several characteristics, including facilities’ physical and social environments, the ability to reach facilities or use services, and healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 fulfillment needs.43 One study defines “accessibility” in five dimensions: approachability, availability, affordability, acceptability, and appropriateness.44 This brief will focus on affordability when discussing the financial inaccessibility of mental healthcare and will consider affordability and financial accessibility as synonymous terms.45, 46
HealthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 services are financially inaccessible if an individual is unable to access healthcare services because they lack the means to afford the required copay or deductible.47 For instance, the average cost of psychotherapy in the US ranges from $100.00–$200.00 per session.48 The average cost of a hospital stay for 5.5 days for bipolar disorder is $4,356.00, and $3,616.00 for a stay of 4.4 days treating depression.49 42% of untreated Americans report cost as a barrier to seeking mental healthThe state or condition of one’s emotional and psychological well-being.9 treatment.50
Q: How does mental healthcare in the US compare to mental healthcare worldwide?
A: The United States has the second highest prevalence of depression among countries, tied with Estonia and Australia at 5.90% of the population.51 Canada and Norway, similarly developed countries, ranked as 13th highest for rates of depression.52 Importantly, rates of depression are likely much higher than these reports, especially in less developed countries where their healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 infrastructures are likely less equipped to identify and treat mental illness.53
In 2011, the United States invested $113 billion in mental healthThe state or condition of one’s emotional and psychological well-being.9 treatment (approximately 5.6% of national healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 spending); in 2010, the US spent approximately 27% of the mental healthcare budget on prescription drugs.54 In 2018, healthcare represented 17.7% of the US economy, more than 3 times what it had been 60 years prior.55 The United States spends more on healthcare than any other comparable developed country, with one source crediting the phenomenon to higher prices rather than greater use of healthcare.56 Researchers assert that while the United States spends the most on healthcare, they do not obtain better health outcomes, and the healthcare growth share in the US economy could be unsustainable.57 The United States market healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 system operates on insurance. Insurance enrollees (or customers) pay a regular premium for reduced healthcare treatment charges. Generally, the higher the premium one pays, the lower the healthcare treatment cost and the lower the premium one pays, the higher the healthcare treatment cost. Health insuranceThe arrangement wherein a company or government agency provides compensation for a specified illness or injury in return for a premium payment.7 offers or packages vary widely; many health insurance companies contract with a network of providers who agree to provide care at subsidized costs for their enrollees. Thus, healthcare providers may accept or not accept certain insurances for subsided costs, and health insurance plans vary in benefits they provide.58, 59
Countries comparable to the US, including Finland, Canada, and Norway, have their own mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 systems in place. Finland provides free mental healthcare and maintains the second highest mental healthThe state or condition of one’s emotional and psychological well-being.9 workforce in Europe; due to the budgeting system of the state, the municipalities, and the Social Insurance Institution, mental healthcare is either low-cost or free. In 2019, Finland directed 9.2% of its GDP toward healthcare—although it is unclear how much of this went toward mental healthcare.60 In Finland’s population of 5.56 million, an estimated 7.12% of the population had a mental illness in 2019.61, 62, 63 In Canada, free mental healthcare services are covered by public health insuranceThe arrangement wherein a company or government agency provides compensation for a specified illness or injury in return for a premium payment.7 unless the provider works in private practice.64 Canada’s mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 approach includes investment and innovation; programs such as community-based services, e-mental health, and increasing access to psychotherapy have improved mental healthcare access and efficiency for the estimated 20% of Canadians affected by mental illness.65 The Canadian federal government invested $994.6 million in mental health care in 2021.66 Norway budgeted €48,000.00 (approximately $50,218.00) per 100,000 individuals in 2017, equating to 6.9% of their total health budget.67 Norway provides community-based mental healthcare;68 its universal healthcare system provides automatic enrollment and is funded by general taxes and payroll contributions.69
Q: What does mental health policy look like in the United States?
A: While various federal legislation and regulation related to improving mental healthThe state or condition of one’s emotional and psychological well-being.9, such as the 21st Century Cures Act (2016), Patient Protection (2010), and the Children’s Health Act (2000),70 this brief will only focus on policy regarding the financial accessibility of mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8, which primarily pertains to the Mental Health Parity and Addiction Equity ActUnited States legislation that requires equal treatment and financing of mental health conditions and substance abuse disorders in insurance plans.16 (2008) and the Affordable Care ActA healthcare reform law established in March 2010. This law is designed with three primary functions in mind: make affordable health insurance available to more people through providing subsidies that lower costs for households with incomes between 100–400% of the federal poverty level; expand the Medicaid program to cover all adults with incomes below 138% of the federal poverty level; support innovative medical care delivery methods directed towards lowering costs of healthcare.2 (2010). While the Affordable Care Act is relevant to discussions on financial accessibility, academia lacks research on the ACA’s effectiveness in practice. Furthermore, while Medicare does legally require mental healthcare coverage, mental healthcare services covered by Medicare are less extensive than their coverage for other services. Many of its services are only covered by mental conditions deemed medically necessary, and those services, as well as others, are limited in the duration of their available access.71 Therefore, this brief will primarily discuss the Mental Health Parity and Addiction Equity ActUnited States legislation that requires equal treatment and financing of mental health conditions and substance abuse disorders in insurance plans.16 (MHPA).
The MHPAUnited States legislation that requires equal treatment and financing of mental health conditions and substance abuse disorders in insurance plans.16 established legal requirements for health insuranceThe arrangement wherein a company or government agency provides compensation for a specified illness or injury in return for a premium payment.7 companies, mandating that insurers provide financial and treatment coverage for mental illness and substance abuse disorders comparable to what is provided for medical and surgical care. Financial and treatment coverage includes deductibles, coinsurance, out-of-pocket expenses, and copayments. However, the MHPA only requires parityThe state of being equal or equivalent.11 if the health insurance plan already provides benefits for mental healthThe state or condition of one’s emotional and psychological well-being.9 and substance abuse disorders. Later, the Enactment of Patient Protection and Affordable Care ActA healthcare reform law established in March 2010. This law is designed with three primary functions in mind: make affordable health insurance available to more people through providing subsidies that lower costs for households with incomes between 100–400% of the federal poverty level; expand the Medicaid program to cover all adults with incomes below 138% of the federal poverty level; support innovative medical care delivery methods directed towards lowering costs of healthcare.2 (ACA) strengthened mental health and substance abuse disorders coverage by mandating treatment coverage for specific plans (plans offered by the state exchanges, Medicaid expansion programs, and individual and small group plans). Additionally, the ACA prohibited yearly and lifetime limits and mandated a federal appeals process for adverse benefits determinations.72 In 2009, before the enactment of the ACA, 30.2 million adults (13.3% of the US adult population) received mental health services during the past 12 months;73 in 2011, after the implementation of the ACA, among 45.6 million adults with any mental illness, 38.2% received mental health services in the past year.74 While millions of Americans obtained mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 and substance abuse disorders coverage by the addition of the ACA, numerous barriers keep many from adequately accessing these services.
Contributing Factors
Inconsistent Execution of the Mental Health Parity and Addiction Equity Act
The ineffective practice of the Mental Health Parity and Addiction Equity ActUnited States legislation that requires equal treatment and financing of mental health conditions and substance abuse disorders in insurance plans.16 contributes to inaccessible mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 in the United States because gaps in legislation and subjectivity lead to ineffective enforcement. Insurers can limit mental healthThe state or condition of one’s emotional and psychological well-being.9 and substance abuse disorders care on a case-by-case basis; thus, insurers maintain the power of determining what is considered “medically necessary.”75 This screening process can further complicate access to treatment because different mental illnesses and disorders maintain varying amounts of stigma associated with the degree of presumed “choice”; for example, insurance companies could choose to medically cover a veteran with PTSD because they would likely be considered victims of events outside of their control that resulted in their debilitating mental illness. In contrast, an insurance company could view someone with anorexia as someone who developed their mental illness by their choice to restrict their eating to lose weight.
Additionally, treatment requirement assessment for mental illness and substance abuse disorders can be difficult to substantiate; for example, one patient who was 5’7” and 100 pounds was denied inpatient treatment for her eating disorder because she was not “underweight enough.”76 In another case, a 14-year-old named Katherine West suffered from major depression, self-mutilation, and bulimia (an eating disorder wherein the individual purges their food).77 Her doctor-prescribed treatment would take 12 weeks in a hospital and cost $50,000.00.78 However, Anthem, her insurance company, would only pay for 6 weeks.79 Anthem argued that Katherine had put on enough weight to be released, but doctors warned that “[Katherine] was desperate to shed those pounds.”80 She was discharged because her insurance company would not pay for further treatment, and later passed away due to continued purging and subsequent heart failure.81 Moreover, studies have shown that insurance denials for mental healthcare occur approximately twice as frequently compared to denials for physical healthcare; researchers found that the most commonly denied mental healthThe state or condition of one’s emotional and psychological well-being.9 treatments were “residential treatment, intensive outpatientOutpatient mental healthcare refers to intensive mental health treatment that does not require an inpatient hospital stay; outpatient services provide patients with intensive mental health services while allowing them to return home at night and continue their daily obligations.10 treatment, psychological rehabilitation, partial hospitalization, home- or community-based therapy, and diagnostic tests.”82 A CBS reporter reviewed several cases wherein doctors, who worked for insurance companies, denied claims by people with mental illness in need of long-term mental healthcare.83 IThe reporter found that the denial rate often exceeded 90% in the cases reviewed.84 Given that mental health issues pose just as serious as physical health issues, this discrepancy in insurance denials disproportionately limits access to mental health services for individuals who need care.
Additionally, studies have found that insurance networks that provide mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 are significantly narrower than for physical and other medical providers; consequently, researchers found that a quarter of individuals could not find a behavioral health“Behavioral health refers to mental health, psychiatric, marriage and family counseling and addictions treatment, and it includes services provided by social workers, counselors, psychiatrists, neurologists and physicians, the National Business Group on Health says. Behavioral health includes mental health and substance use, encompassing a continuum of prevention, intervention, treatment, and recovery support services.”4 specialist in their network.85 In comparison, just 10% were unable to find a physical health specialist in their network, which results in higher out-of-pocket costs for mental healthThe state or condition of one’s emotional and psychological well-being.9 care.86 Many of these Mental Health Parity and Addiction Equity ActUnited States legislation that requires equal treatment and financing of mental health conditions and substance abuse disorders in insurance plans.16 shortcomings illustrate the inaccessibility of mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 for those who are already insured; many Americans remain uninsured, thereby having to pay out-of-pocket for treatment or forgo it entirely.87 Thus, because of the barriers to achieving parityThe state of being equal or equivalent.11 of mental health coverage to physical healthcare, as well as the inefficiencies and shortcomings in enforcement and monitoring of insurers, many Americans, both insured and uninsured, are unable to access needed mental healthcare treatment.
Employment-Based Coverage
This discussion particularly impacts low-income individuals due to their higher likelihood of developing poor mental healthThe state or condition of one’s emotional and psychological well-being.9,88 increased financial vulnerability, and reduced ability to address high mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 costs. As such, in this section, this brief will highlight disparities in healthcare access by socioeconomic statusThe social status or standing of an individual, typically measured by education, income, and occupation.15, given its relevance to employment-based coverage.
Individuals with incomes less than twice the federal poverty threshold to meet basic needs are considered low-income.89 For those considered to be in poverty, the total family income must be less than the federal poverty threshold for that family.90 In 2020, there were 37.2 million people in poverty, an approximate 3.3 million increase from 2019.91 From December 2021 to February 2022, overall poverty increased to 14.4% in the United States, an increase of 6 million more individuals in poverty from December to February.92 Having a low-income is associated with several lifetime mental disorders and suicide attempts;93 approximately 8.7% of individuals living below the poverty line reported severe psychological distress.94
Because the United States primarily uses employers as providers of health insuranceThe arrangement wherein a company or government agency provides compensation for a specified illness or injury in return for a premium payment.7 coverage for their employees and dependents,95 low-income families are disproportionately disadvantaged in obtaining healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 insurance and thus accessing mental healthcare. First, low-income individuals are generally employed in part-time jobs; among people employed for 27 weeks or more in 2018, 2.8% of those employed full-time were the working poor, compared to 11.1% of part-time workers.96 Studies have shown that wages and benefits are almost always lower for part-time workers: women were 88% less likely, and men were 86% less likely to have a pension or health insurance from their part-time employment.97 Second, low-income working parents are more likely to have employment in service occupations.98 Service occupations, such as childcare workers, cosmetologists, and lobby attendants,99 are more likely to have lower wages, have fewer opportunities to attain full-time employment, and are less likely to provide benefits such as health insurance.100 According to a report on occupational benefits in the US, 49% of people in service occupations had access to medical care benefits (versus 89% of management and related occupations), and 33% of service occupations had access to life insurance benefits (versus 80% of management and related occupations).101 Life insurance benefits include paying off debt, such as medical bills after an individual has passed away, and paying for one’s funeral and cremation expenses; life insurance benefits help create a financial safety net for the deceased’s beneficiaries.102 Medical care benefits, such as life and health insurance, are disproportionately inaccessible to low-income individuals because of employment. Working low-income individuals are more likely to be employed in occupations that do not provide healthcare insurance, which is the primary source of health insurance providers in the United States.
Moreover, employed low-income individuals receive fewer occupational benefits than their middle-income peers. Research has repeatedly shown that uninsured populations are less likely than insured populations to receive preventative care for major health conditions and chronic diseases: 21% of uninsured nonelderly adults disclosed going without needed healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 in the past year, while 7% with public coverage and 4% with private coverage reported going without needed healthcare in the past year.103 Thus, uninsured nonelderly adults were approximately 5–6 times more likely than those with private coverage and 3 times more likely than those with public coverage to go without needed healthcare. Employed low-income families with at least one full-time worker were less likely than middle-income families to have health insuranceThe arrangement wherein a company or government agency provides compensation for a specified illness or injury in return for a premium payment.7 provided by an employer (49% versus 77%); relatedly, many low-income families reported having to postpone needed medical care because they lacked health insurance or money.104 Therefore, because the United States primarily focuses on employer-based health insurance providers, low-income Americans, who are more likely to be employed in occupations that do not provide health insurance, are disproportionately unable to access mental and physical healthcare services.
High Healthcare Expenses
Many Americans cannot access healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 in the United States because of its high out-of-pocket costs, or costs that an individual must pay without insurance’s assistance around the time of treatment. An overview of mental healthThe state or condition of one’s emotional and psychological well-being.9 inpatient treatment centers found that prices for psychiatric residential treatment facilities ranged from $10,000.00–$60,000.00 per month.105 Another report found that the average cost of an inpatient hospital stay was $11,700.00 in 2016 (approximately $13,200.00 in 2021); moreover, the authors disclosed that “full charges are likely about 4 times higher than the reported [costs].”106 These high healthcare costs create a financial barrier for many Americans suffering from mental illnesses, which can be chronic, long-term mental conditions.
Photo by Dziana Hasanbekava
The rapidly increasing US healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 costs have made healthcare financially inaccessible for families in America and economically strained governments and businesses. For example, the New York Times reported that an average daily hospital cost was $127.00 in 1980;107 today, an average 3-day hospital stay costs approximately $30,000.00 ($10,000.00 a day).108, 109 Nationwide, a complex hospitalization for COVID-19 costs $317,810.00.110 Thus, while Americans are charged with substantially increased healthcare charges, most Americans’ wages' purchasing power has stagnated since 1978.111 Therefore, Americans who need medical care must pay significantly increased costs with wages that have not increased proportionally. Because the United States’ healthcare and health insuranceThe arrangement wherein a company or government agency provides compensation for a specified illness or injury in return for a premium payment.7 costs are so expensive—and disproportionately more expensive than any of its comparable developed countries—mental healthcare remains inaccessible.
Negative Consequences
High Suicide Rates
Inaccessible mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 leads to higher suicide rates because, without preventative mental healthThe state or condition of one’s emotional and psychological well-being.9 services, individuals with mental health challenges are more vulnerable to suicide. The US maintains a relatively high suicide rate.112 According to a 2020 report by the Centers for Disease Control and Prevention, suicide was the twelfth leading cause of death; there were about twice as many suicides (45,979) in the United States as homicides (24,576) in 2020.113 The total age-adjusted“Age-adjusted” data allow populations with different age structures to be statistically compared; this is often applied to health outcomes measurements.3 suicide rate in the United States was 10.4 (per 100,000 people) in 2000 and increased to 13.5 in 2020.114 While high suicide rates suggest a high need for mental health services, few individuals needing services for suicidal thoughts reported receiving them due to inaccessibility. Researchers reported that 34.8%–45.5% of American adult survey participants reported needing mental health services but did not receive them during their evaluation period.115
Photo by Kat Smith from Pexels:
While suicide rates seem to be increasing, researchers also reported that mental healthcare utilization among those who attempted suicide has not increased, which suggests a need for service accessibility expansion.116 A systematic review and meta-analysis of data published from 2000–2017 reveal that only 18.3% of individuals who committed suicide had an inpatient mental health stay, only 26.1% acquired outpatientOutpatient mental healthcare refers to intensive mental health treatment that does not require an inpatient hospital stay; outpatient services provide patients with intensive mental health services while allowing them to return home at night and continue their daily obligations.10 mental health services, and only 25.7% had both inpatient and outpatient mental health services.117 Thus, while rates of suicide are increasing, access to services is continually inadequate.118, 119 Researchers examining risk and suicide attempt reduction in subjects who had attempted suicide subjected a control group to TAU (treatment as usual) and a treatment group to intervention, which consisted of risk screening by emergency department physicians, discharge resources, and post-emergency department phone calls to reduce suicide risk. Their results indicated that participants in the intervention had significantly fewer suicide attempts than participants in TAU.120 Thus, access to subsequent mental health services significantly reduced their likelihood of re-attempting suicide. Access to mental health preventative services helps to reduce suicide attempts, while inaccessibility to these services helps to aggravate suicide rates.
Greater Economic Burden
The inaccessibility of mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 negatively impacts the economy by impacting working benefits, increasing debt, reducing productivity, and damaging GDP. The rapid augmentation in health insuranceThe arrangement wherein a company or government agency provides compensation for a specified illness or injury in return for a premium payment.7 premiums can cause firms to stagnate wages, lessen health insurance benefits, or require employees to work more hours to accommodate rising costs. Researchers found that when health insurance premiums increase, firms budget approximately two-thirds of the increase by reducing workers’ wages and one-third by reducing benefits.121 Researchers found that during their study period, insurance coverage decreased by 3.1% while premiums grew by 53%; they concluded that more than 50% of the decline in coverage rates was attributable to the rise in health insurance costs.122 Firms unable to compensate for the rise in health care costs may decrease employment or replace full-time employees, who are eligible for benefits, with part-time employees, who are not eligible for benefits.123 Scholars assert that as more health insurance costs are shifted to consumers, they may relinquish insurance coverage or reduce their utilization of healthcare services.124 One study combined data from various sources to illustrate the impact of rising healthcare costs on a hypothetical median-income married couple with two children, all covered by employer-provided insurance in the US; their examination compared the family’s healthcare costs from 1999–2009, while tracking income with healthcare costs according to the Consumer Price Index.125 Researchers found that, despite the growth in the family’s income through the years, rising healthcare costs largely consumed their income. If the US healthcare costs had not outpaced the Consumer Price Index, an average American family would have $450.00 more per month (more than $5,000.00 annually).126 Thus, rising healthcare costs burden consumers’ income.
Because high healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 costs burden consumers’ income, consumer debt is also negatively influenced. Medical debt is a relatively common phenomenon in the United States; the KFF Health Care Debt Survey issued in the United States found that 4 in 10 adults had healthcare debt and that low-income individuals and uninsured individuals are more likely to report having medical debt.127 The Consumer Financial Protection Bureau found that approximately $88 billion in healthcare debts are represented in Americans’ credit reports, noting that the actual total of medical debt is likely higher due to the absence of those without credit reports and the medical debt not available to consumer reporting organizations.128 One study found that high medical debt was associated with subsequent housing problems for low- and middle-income individuals: in a survey of low- and middle-income individuals, half of the respondents disclosed having healthcare debt, and a quarter of those also reported experiencing housing issues because of their healthcare debt.129 Another survey showed that approximately a third of respondents described that their healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 expenses contributed to their current credit card debt. In households with healthcare debt, the average credit card debt was substantially higher than in households without medical payments contributing to their overall credit card debt.130 Researchers conclude that medical debt can drain family savings and inhibit their access to future medical resources and services.131
High healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 costs also negatively impact consumers by reducing productivity and damaging GDP. Scholars estimate that poor mental healthThe state or condition of one’s emotional and psychological well-being.9 and consequentially reduced productivity cost the global economy approximately $2.5 trillion per year in 2010; researchers project that cost to increase to $6 trillion by 2030.132, 133 Inaccessible mental healthcare and poor mental health produce both inefficiency and high cost in the US healthcare system, as well as indirect costs, such as reduced contributions to the market and reduced volunteering.134, 135 For every dollar invested in treatment for depression and anxiety, there is a $4.00 return in improved health and productivity.136 Financial inaccessibility to mental healthcare perpetuates poor mental health, which reduces worker productivity and damages the overall economy. One study concluded that each poor mental health day was associated with a 1.84% lower per capita real income growth rate ($53 billion less total annual income) in the US for 2008–2014.137 The direct and indirect global economic costs of mental disorders were estimated at approximately at $2.5 trillion in 2010.138 Interestingly, the indirect costs ($1.7 trillion) were significantly higher than the direct costs ($800 billion), in contrast to other prominent human illnesses, such as cancer and cardiovascular diseases.139 Thus, because inaccessibility to mental healthcare perpetuates poor mental health, worker productivity is lowered, and GDP is damaged therefore maintaining a significant, negative impact on national and global economies.
Poor Physical Health
Because mental illness is strongly correlated to poor physical health, inaccessibility to mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 also represents the danger of increased likelihood of poor physical health ailments. Studies found that mental illness is associated with a greater occurrence of cancer, cardiovascular disease, obesity, asthma, epilepsy, and diabetes.140 Researchers noted in one study that individuals with serious mental illness can have cardiovascular disease 3.6 times more frequently than those in the general population.141 In England, a comparably developed country to the United States, 37.6% of individuals with serious mental illness also have a long-term physical ailment, compared to 25.3% with no or few symptoms of poor mental healthThe state or condition of one’s emotional and psychological well-being.9.142 Moreover, individuals with chronic physical health conditions experience depression and anxiety at twice the rate of the general population.143 The CDC reports that depression increases the likelihood of multiple types of physical illnesses, such as heart disease and stroke. Therefore, unmet mental health needs to increase the risk of developing these negative physical outcomes.
Research has overwhelmingly documented that having access to mental and physical healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 promotes longevity; scholars found that adequate access to healthcare better enables individuals to manage their health challenges and benefits positive health outcomes,144 and the lack of universally accessible healthcare “undoubtedly” reduces life expectancy and increases mortality.145 One study found that limited access to healthcare was accountable for approximately 10% of premature deaths or other negative health consequences;146 moreover, in areas where women have access to healthcare, maternal deaths are reduced, and women’s longevity is increased.147 Individuals with serious mental illnesses have a significantly reduced life expectancy compared to the general population. Because access to mental healthcare helps to alleviate the negative effects of serious mental illness, adequate access to mental healthcare helps to promote longevity for those with serious mental illness.
Best Practices
Safety Net Hospitals
Safety net hospitalsA type of medical center in the United States that, by legal obligation, provides healthcare for individuals regardless of their insurance status or ability to pay; these hospitals typically provide services disproportionately to low-income and marginalized populations.12 are medical centers in the United States that are legally obligated to provide healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 to individuals, regardless of their insurance coverage or ability to pay.148 These organizations typically provide services to low-income and marginalized populations, who are more likely to be those who are uninsured or underinsured; thus, their presence and functioning in low-income communities and to uninsured and underinsured individuals proves essential to the mental healthThe state or condition of one’s emotional and psychological well-being.9 and well-being of these Americans.149, 150 The methodology by which researchers define what qualifies as a safety-net hospital varies widely, but many utilize its Medicaid disproportionate share hospital (DSH) status as a defining factor. In 2018, one study defined what qualified as a safety-net hospital by DSH status and facility characteristics; they calculated 640 and 1194 safety-net hospitals in the United States by these two factors, respectively.151, 152 Another study found that in 2015, safety-net hospitals in states that had expanded Medicaid had more than double the level of uncompensated care costs and Medicaid income compared to other hospitals.153 In addition to providing financial accessibility, safety-net hospitals typically provide services such as interpretation, assistance with insurance, and case management.
Since 1986, the federal government has provided monetary compensation for safety net hospitalsA type of medical center in the United States that, by legal obligation, provides healthcare for individuals regardless of their insurance status or ability to pay; these hospitals typically provide services disproportionately to low-income and marginalized populations.12; however, the ACAA healthcare reform law established in March 2010. This law is designed with three primary functions in mind: make affordable health insurance available to more people through providing subsidies that lower costs for households with incomes between 100–400% of the federal poverty level; expand the Medicaid program to cover all adults with incomes below 138% of the federal poverty level; support innovative medical care delivery methods directed towards lowering costs of healthcare.2 amended this, thereby reducing government compensation payments to counteract a growing insured low-income population.154 Researchers comparing non-safety-net hospitals to safety-net hospitals found that the latter generally had more staffed beds, more full-time staff, and admitted more patients.155 Moreover, studies have found that safety-net hospitals are more likely to be situated in urban areas; 82.5% of safety-net hospitals were located in urban areas compared to 77.4% of non-safety-net hospitals.156
Safety-net hospitals are generally situated in low-income, disadvantaged communities and often serve a high proportion of racial and ethnic minorities; these circumstances create a restricted resource environment from which safety-net hospitals operate.157 Because safety net hospitalsA type of medical center in the United States that, by legal obligation, provides healthcare for individuals regardless of their insurance status or ability to pay; these hospitals typically provide services disproportionately to low-income and marginalized populations.12 are at the forefront of absorbing unreimbursed medical expenses of uninsured or underinsured, they commonly become bankrupt or bought out due to the inability to finance operations because of deficient revenue from self-pay patients.158 For example, out of 20 rural hospitals that closed in 2020, at least 9 were safety-net hospitals.159 Additionally, state and local budget cuts to Medicaid especially harm safety-net hospitals’ functionality, creating a greater risk of closure or privatization.160 Moreover, some speculate that the federal Hospital Value-Based Program (VBP), which rewards and adjusts payments to hospitals based on performance, could negatively impact safety-net hospitals.161 While safety-net hospitals fare equally well with non-safety-net hospitals in Performance Improvement measures, safety-net hospitals tend to score lower than non-safety-net hospitals on patient experience metrics;162 thus, the VBP penalizes them with Medicaid payment cuts.163 In 2014, 63% of sampled safety-net hospitals received reduced aid under the VBP, compared to 51% of all other sampled hospitals.164 Because the VBP program can withhold 2% of participating hospitals’ Medicaid payments, safety-net hospitals, which operate on constrained resources and serve particularly vulnerable and at-risk patients, the VBP could lose federal aid.165 Moreover, researchers found that the percentage of patients reporting high scores on patient experience increased before the VBP began (an annual change of 1.84%; 95% Confidence Interval, 1.73%–1.96%), and then increased at a slower rate after the VBP implementation (an annual change of 0.49%; 95% Confidence Interval, 0.45%–0.53%); similar patterns were observed for non-safety-net hospitals as well (before the VBP implementation, an annual change of 1.84%; 95% Confidence Interval, 1.77%–1.90%; in contrast, after the VBP began, an annual change of 0.42%; 95% Confidence Interval, 0.41%–0.45%).166 Safety-net hospitals are pertinent sources of financially accessible mental healthcareThe maintenance and improvement of health through prevention, diagnosis, treatment, cure of illnesses and injuries, and any other physical and mental ailments.8 for disadvantaged communities. Because they maintain financial and resource vulnerability due to their absorption of a high market share of uncompensated and under-compensated healthcare costs, as well as monetary penalties introduced by the VBP, safety-net hospitals maintain financial insecurity, which can inhibit resource accessibility and effect patient experience.
Preferred Citation: Lasswell, Sophie. “Financial Inaccessibility of Mental Healthcare in the United States.” Ballard Brief. October 2022. www.ballardbrief.byu.edu.
Viewpoints published by Ballard Brief are not necessarily endorsed by BYU or The Church of Jesus Christ of Latter-day Saints